Why GLP-1 Coverage Matters
GLP-1 weight loss medications, including Wegovy and Zepbound, are transforming the conversation around employee health benefits. These prescription drugs are popular with members who see them as essential for managing weight and improving health outcomes. Meanwhile, for health plans, they represent a significant financial challenge due to their rapid increase in utilization.
Current Employer Trends
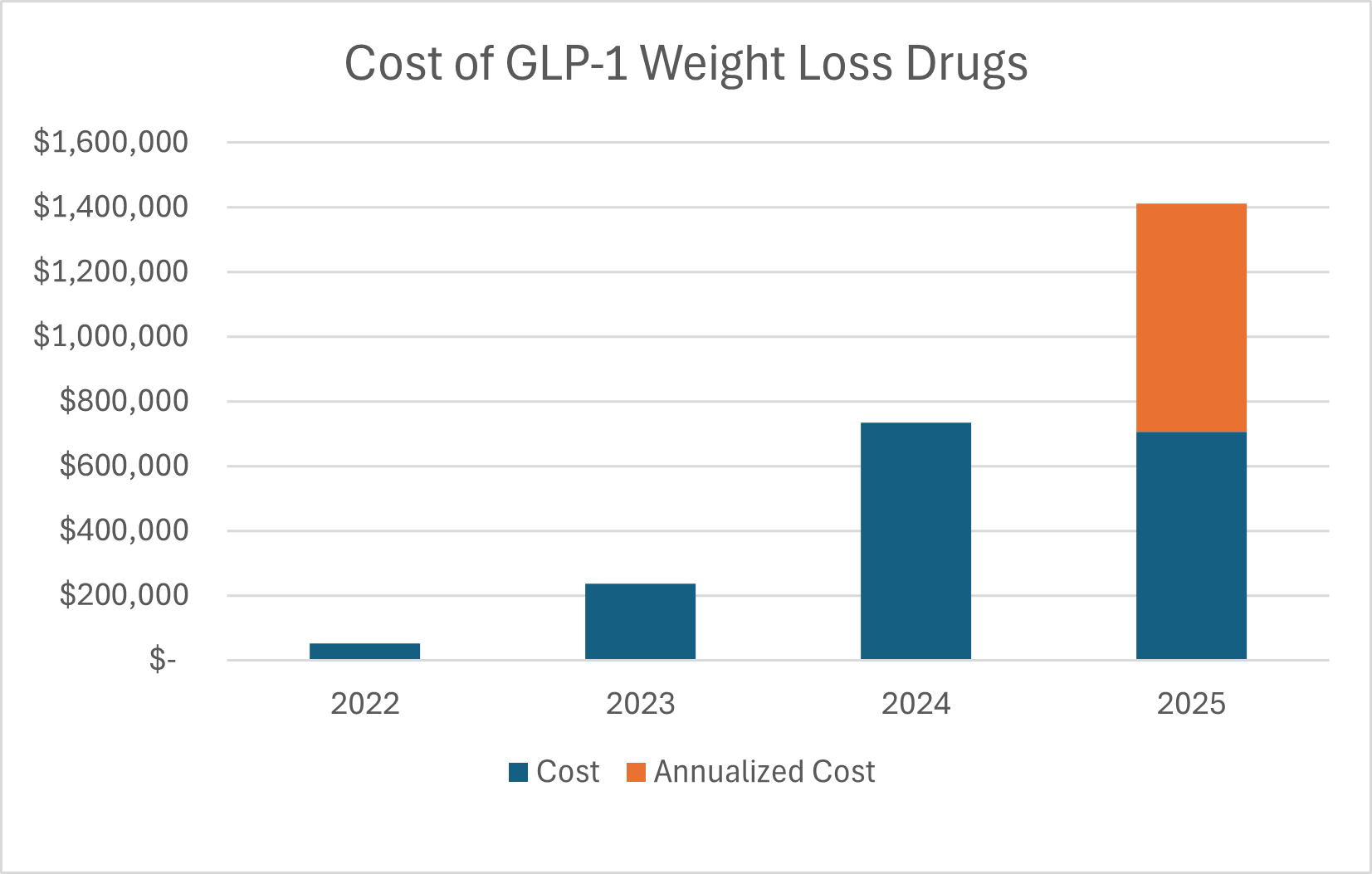
Since these medications gained popularity, utilization (and cost) has surged for plan sponsors. Below is a table of the cost of GLP-1 weight loss drugs over the last few years for one of our employer clients. For both 2023 and 2024, the costs more than doubled compared to the prior years. To date in 2025, GLP-1 weight loss medications accounted for over 10% of the prescription drug plan costs (prior to rebates) for this plan. This trend is common – or even worse – among many other employers that cover these medications.
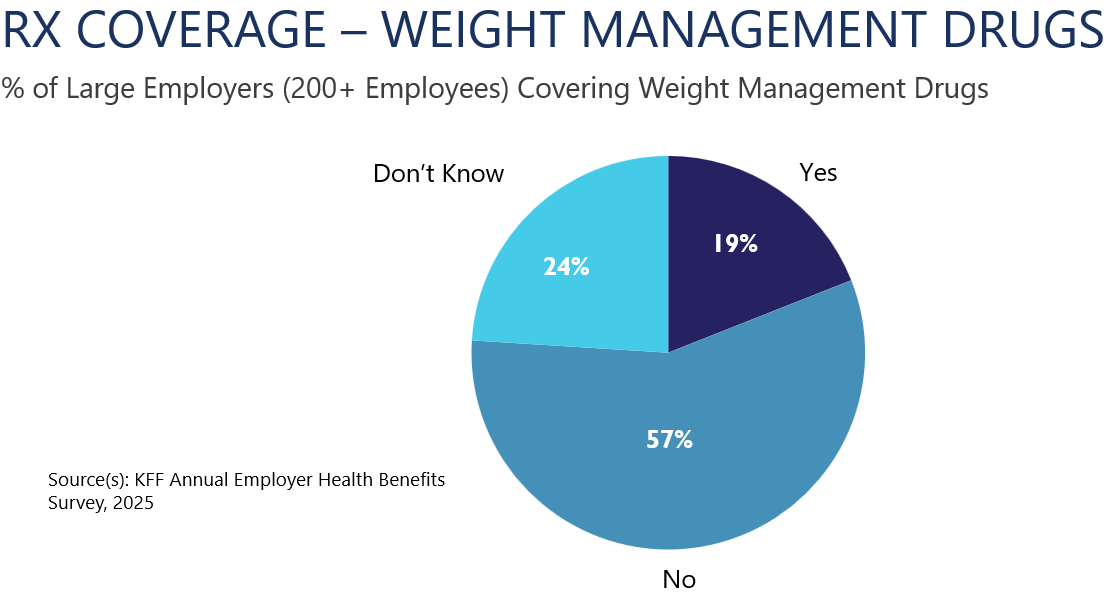
It is important to note that weight management drugs are not currently required to be covered by your health plan. Coverage decisions vary widely among employers. According to the 2025 Kaiser Family Foundation Annual Benefit Survey:
- 19% of large employers (200+ employees) cover GLP-1 weight loss medications,
- 57% do not cover them, and
- 24% are uncertain about the coverage status for their health plan.
Given the significant cost implications, every health plan should review its coverage strategy and make an informed decision moving forward.
Questions to Ask
Coverage decisions should align with fiduciary obligations to balance cost with access to care. Keep in mind that the questions (and potential options) may change depending on how your plan is funded (fully insured, self-funded, etc.), the goals and objectives of your benefit offerings, and the current/projected utilization of these prescription drugs for your plan. Here are some key questions to ask your plan advisors, insurers, and PBMs (pharmacy benefit managers):
Coverage Status:
- Does my plan cover GLP-1 weight loss drugs (or any other weight loss drugs)?
- Does my plan provide any other options to help treat obesity?
- What are the pros and cons of covering these prescription drugs? Understand the debate regarding:
- short-term cost,
- efficacy, and
- weight loss impact on longer-term plan costs.
Cost Management:
- How much is my plan paying for these medications? Are rebates offsetting any of these costs?
- How much are our plan members paying for these medications through our health plan?
- Can employee cost-sharing (copays, coinsurance, deductibles) be adjusted? How would that impact pricing and rebates?
Utilization Controls:
- Are there eligibility restrictions (including prior authorizations and/or utilization management programs) in place?
- Can additional restrictions be put in place without excluding coverage entirely? How would that impact pricing and rebates?
If Coverage Is Not Offered:
- What options exist for members to access these medications outside the health plan and at what cost?
- Are there alternative options/resources (carve-out options, third-party vendors, HRAs) to support employees without direct coverage through our insurance carrier / PBM? How does this cost and access to coverage compare to direct coverage?
Next Steps for Fiduciaries
Being informed about GLP-1 weight loss prescription drugs and how they affect your healthcare plan is critical. For 2026 and beyond, we recommend all plan sponsors:
- Review current coverage and utilization data,
- Evaluate options and model cost scenarios, and
- Ensure decisions align with fiduciary responsibilities and corporate benefit goals and objectives.
Conrad Siegel delivers big firm capabilities, with a small firm feel. We strive to simplify complexity for our clients. We are partners who prefer rolling up our sleeves, solving complex problems, and taking the administrative burden off your plate. Should you want to explore this further, please do not hesitate to contact us to review your plan strategy.


